Many healthcare workers may lose access to COVID vaccines
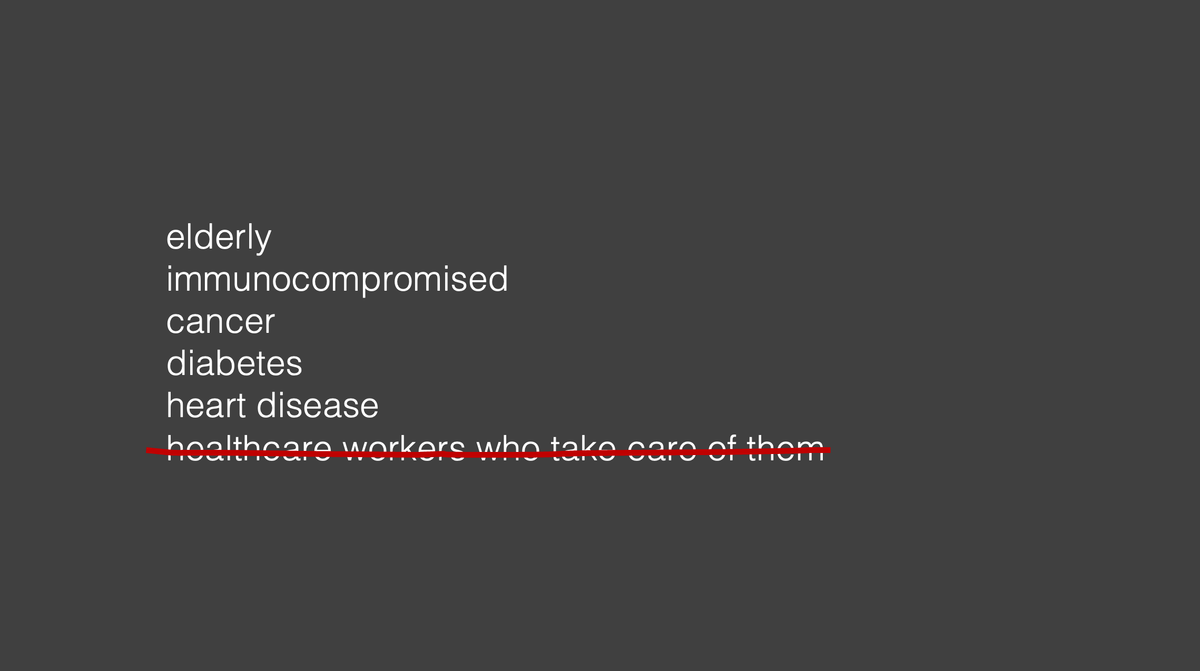
This week, a new proposal for COVID vaccines was announced that—if implemented—will likely mean many healthcare workers like me will no longer have access to COVID shots.
Two new FDA appointees announced the change via an opinion article in the New England Journal of Medicine: COVID boosters will only be approved for the high risk, and it's back to the drawing board (i.e. new randomized controlled trials) for everyone else. Up until now, COVID booster shots have been approved (which determines if it's available and covered by insurance) for everyone older than 6 months.
This new proposal is both impractical and foolish, and as a healthcare worker, is extremely frustrating. I routinely walk into the rooms of patients who have functionally zero immune system. This change makes it harder to keep patients safe.
What they're proposing
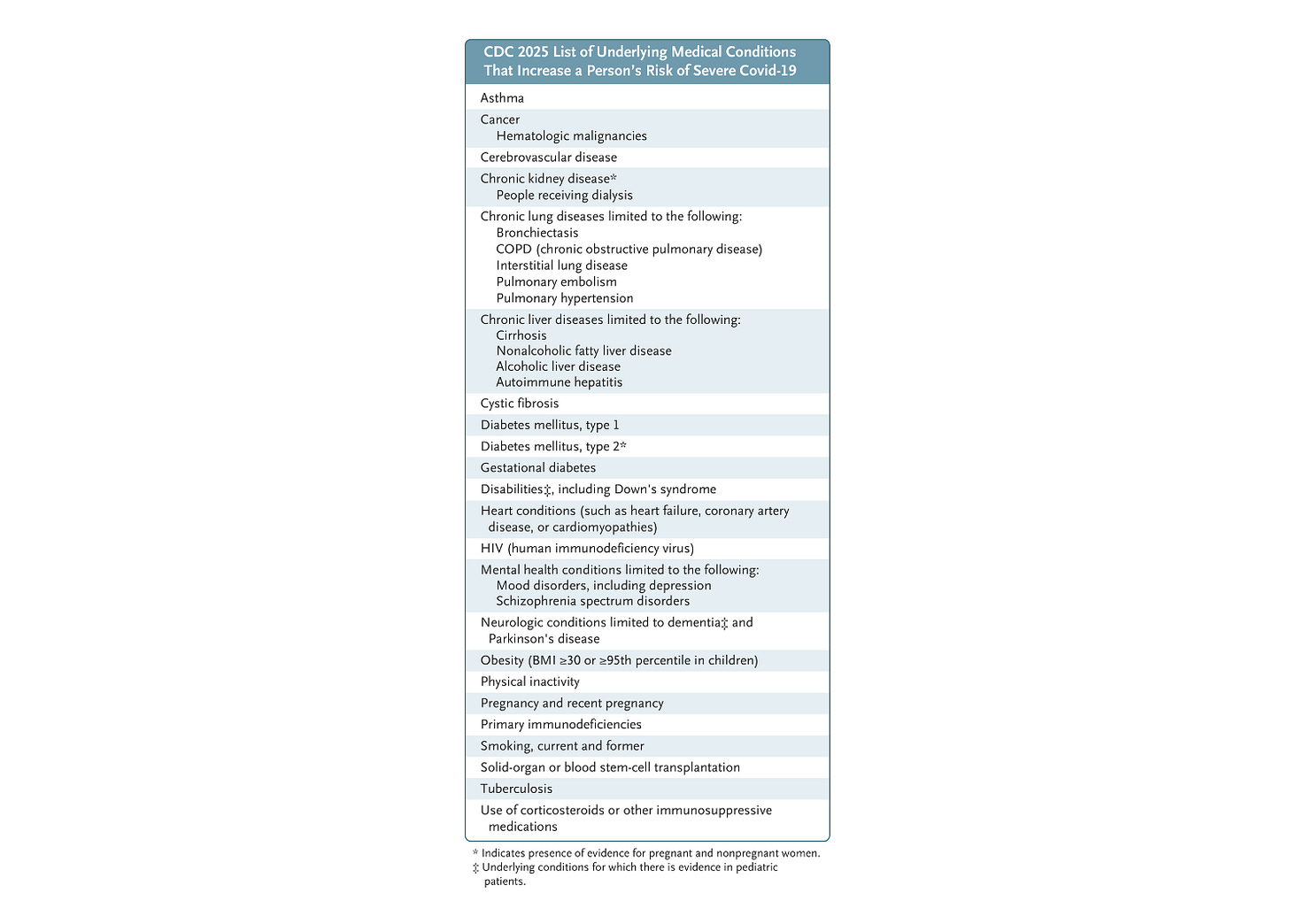
The new proposal would approve COVID vaccines for two groups of people:
- Everyone over age 65
- Those over age 6 months with an underlying condition (see list below).
There is no exception listed for healthcare workers. Unless they announce a change to that policy, that means as a young, healthy doctor, I would not be eligible (though I suppose I could take up smoking).
For everyone else, they require running new randomized controlled trials prior to FDA approval, arguing that people now have more immunity to COVID so the original clinical trials aren't valid anymore.
While this may sound like a reasonable idea on the surface, it is not.
Annual vaccine updates are different than new vaccines
Randomized controlled trials (RCTs) are fully appropriate for new vaccines. Contrary to recent implications, RCTs are conducted for all new vaccines, including the COVID vaccines.
But annual vaccines are different. For annual vaccines like the flu shot and now COVID shots – which are updated to match the latest circulating strains – running new RCTs for vaccine updates is profoundly impractical. By the time you 1. figure out the circulating strain, 2. update the vaccine to match the strain, 3. design the study and get approval, 4. enroll enough people, 5. wait for some of those people to catch COVID so you have data, and 6. analyze and publish the results, it's already next year, and that year's strain is gone.
Instead, annually updated vaccines like the flu shot rely on observational and immunological data, which can be collected much faster. If pharma declines to run these expensive and largely impractical studies, according to this new proposal, the FDA won't let healthy doctors like me have updated COVID shots.
As an ER doc, here's why I've gotten a COVID shot every year
As someone who is young and healthy, my risk of dying from COVID is quite low. Fear of ending up in the ICU or dying from COVID is certainly not what drives me to get vaccinated every year – here's why I do it:
- To protect my patients. COVID is extremely contagious. I do my best to reduce transmission (N95, gloves, washing my hands, etc.), but no single protective measure is 100% perfect. This includes COVID boosters, which offer partial, not complete protection. But when you are surrounded by high risk patients every day at work, that partial protection adds up — especially when that boost in immunity is timed to occur when COVID is spreading (i.e. respiratory virus season). If I show up to work with COVID without knowing it, I could easily expose dozens of high risk patients in one shift. For some of them, that may mean they never get to go home.
- Protection against long COVID. Hospitalization and death aren't the only risks. Reducing the risk of catching COVID also means reducing the risk of long COVID, which can be debilitating for even young healthy adults.
- As a healthcare worker, it's really nice to not get sick. Getting COVID in residency means being exhausted on the couch for a week, having your friends get called in to cover your shifts, and often spending months making those shifts up. When your workplace involves sick children coughing into your eyeballs, it's nice to reduce the risk of that happening with a simple shot.
Other countries let their healthcare workers get vaccinated
The authors of the new proposal argue their new COVID vaccine guidelines are more in line with recommendations in other countries, but that's not entirely true. While many other countries do make more targeted recommendations for COVID boosters emphasizing importance for high risk groups, many still allow lower risk groups to access COVID shots if they would like them, with some specifically mentioning healthcare workers as eligible.
We have processes in place to evaluate changes to vaccine recommendations. This isn't it.
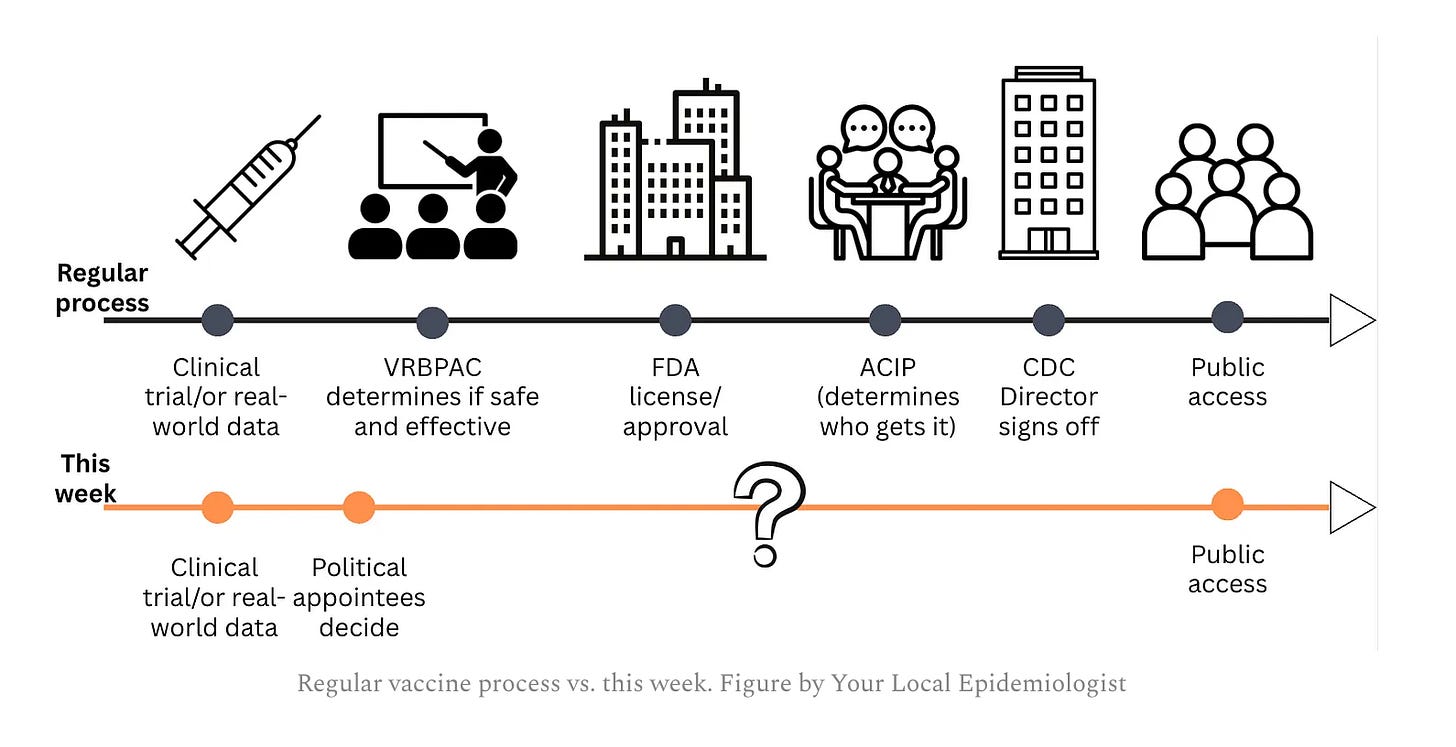
Perhaps the most concerning part about this proposal is the way it was done – via an opinion piece. Normally, vaccine recommendations are carefully assessed and deliberated every year through a multi-stage process involving many different people. Now, two new FDA appointees appear to be steamrolling over that process (read this excellent article for more details).
The path back to trust
There are valid criticisms to be made over how COVID vaccines were handled during the pandemic, with many people feeling angry that the government pushed vaccines on people who didn't want them. Ironically, now we have the same problem in the opposite direction: the government is trying to take vaccines away from people who want them, using unreasonable standards of evidence as their excuse.
The authors of this opinion article argue these changes will help restore trust in the COVID vaccines, believing that new RCTs are the path to regaining trust. As someone who has spent far too much time writing about COVID vaccines, I am dubious. The original COVID vaccine RCTs were frequently misinterpreted and attacked, and any new RCTs are likely to be treated the same way. More data often doesn't fix distrust – the rumor that MMR vaccines cause autism started with a tiny (fraudulent) study of 12 children, but even studies of over a million kids showing no connection haven't assuaged fears.
Unfortunately, I think we are in the same position with the COVID vaccines – when rumors aren't rooted in data, more data is unlikely to help.
Kristen Panthagani, MD, PhD, is completing a combined emergency medicine residency and research fellowship focusing on health literacy and communication. In her free time, she is the creator of the medical blog You Can Know Things and author of Your Local Epidemiologist’s section on Health (Mis)communication. You can subscribe to her website below or find her on Substack, Instagram, or Bluesky. Views expressed belong to KP, not her employer.