The birth dose: why are babies immunized against hepatitis B so early?
RFK Jr’s vaccine panel is meeting this week, and there is widespread concern they may vote to remove the first vaccine on the childhood immunization schedule: the birth dose of the hepatitis B vaccine.
Currently, it's recommended that newborns receive the first dose of the hepatitis B vaccine series within 24 hours of birth.
There has been some confusion and genuine questions about this vaccine from parents of newborns, so here’s a quick breakdown on hepatitis B immunization and why it’s started so early.
What is hepatitis B?
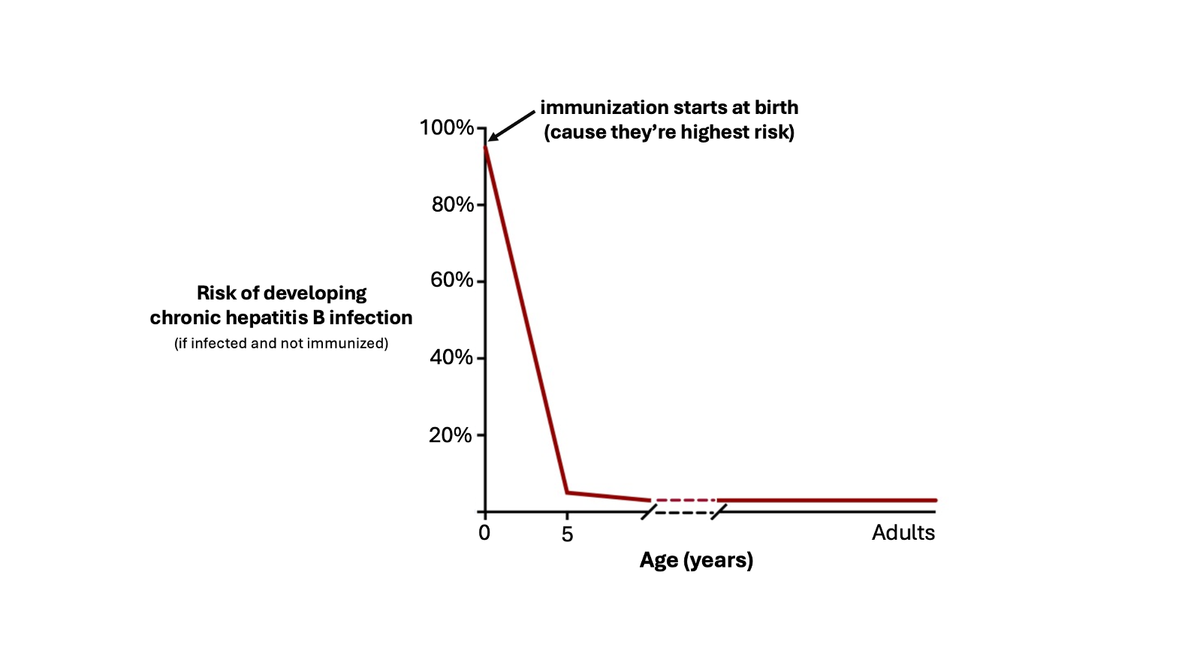
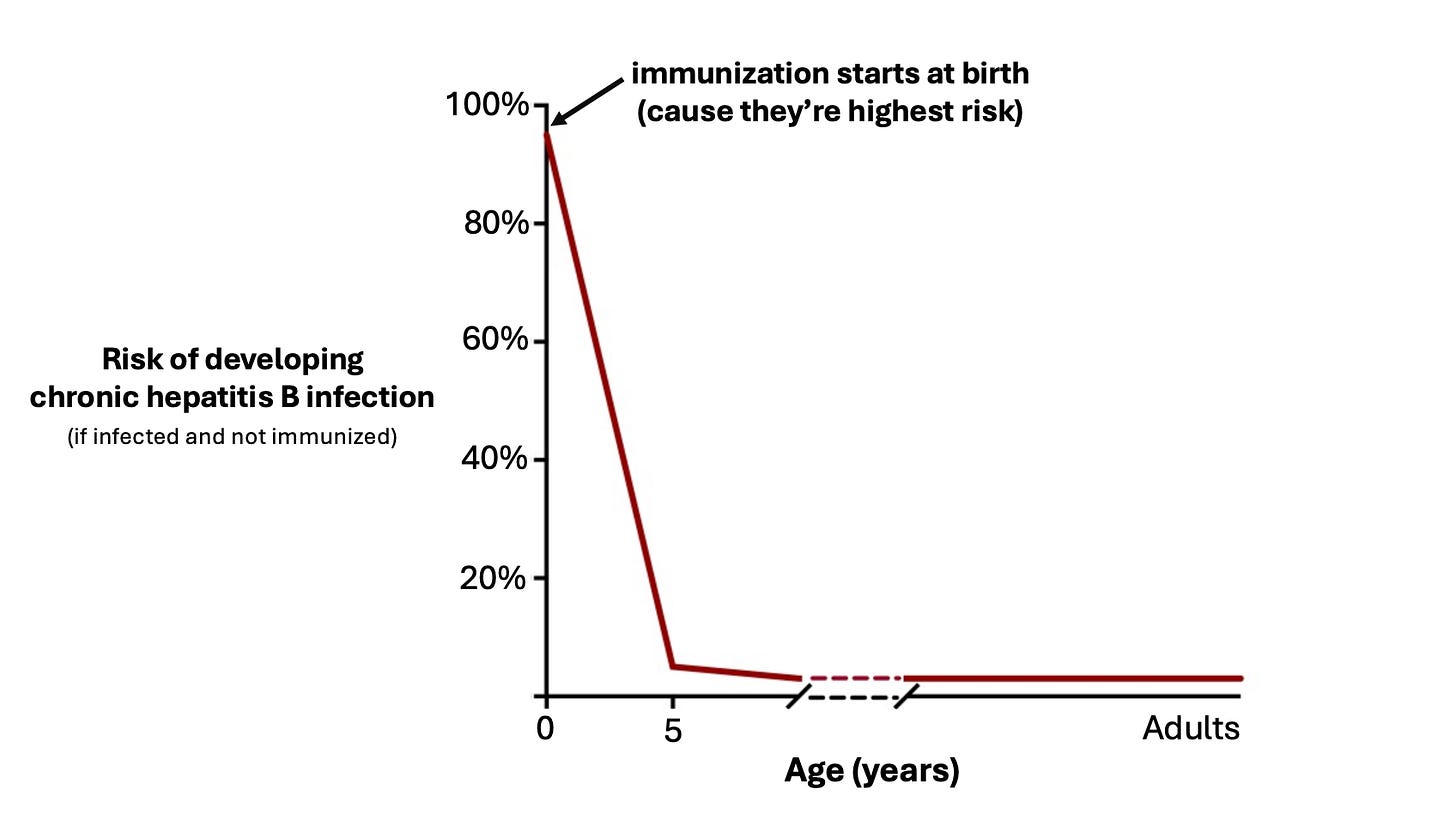
Hepatitis B is a virus that destroys livers. Infants are at highest risk of catching it — when babies are exposed at birth or early infancy, about 90% go on to develop chronic liver infection compared to a 5-10% risk if exposed as an adult. This is why the vaccine is given so early — early in life is the highest risk period.
If a baby catches it, symptoms usually don’t show up right away, and parents often don’t know their child has caught it. Over time, the virus causes chronic inflammation in the liver which can lead to severe liver damage (cirrhosis), liver cancer, liver failure, and for some — death. About 25% of babies who develop chronic infection will die from liver disease later in life.
Is chronic liver infection that big of a deal?
Yes. One thing medical school teaches you is a very strong appreciation for the liver. It performs a whole host of functions from detoxification to synthesis of proteins for blood clotting to glucose regulation. It is called a ‘vital organ’ for a reason — some of the sickest patients who come to the hospital are patients who have chronic liver disease. As an ER doctor, I can assure you — you don’t want to mess with the liver.
How is hepatitis B transmitted?
People most often know about the ‘high risk’ routes of transmission for hepatitis B — from mom to baby at birth, sexual contact, IV drug use, etc.
But these aren’t the only ways it can spread. It is a very hardy and very infectious virus. It can spread through even microscopic amounts of blood and can live on surfaces for days. This means things as simple as sharing tooth brushes or contact with a cut or scrape can transmit it.
Why is the vaccine given to all babies at birth, not just those with high risk moms?
This is a common and very reasonable question. And here's the answer: if we only gave the vaccine to babies of known ‘high risk’ moms, we would end up missing a lot of infections, and every year babies would fall through the cracks and end up with damaged livers. Here’s why:
- ‘High risk’ routes aren’t the only way of catching it. IV drug use and sexual contact aren’t the only ways hepatitis B spreads. Over a quarter of new hepatitis B cases detected in 2022 had no known risk factor or exposure.
- Many people who are infected don’t know it — if we rely on moms to self-report hepatitis B infection, we will miss many cases. It’s estimated about half of people in the US with hepatitis B don’t know they have it.
- Screening isn’t a perfect tool. While screening moms for infection during pregnancy is highly recommended, inevitably not every mom is screened (and some may catch it after screening), leading to missed infections. About 12% of mothers with commercial insurance and 16% of mothers with medicaid aren’t screened appropriately, not to mention mothers who don’t have insurance for prenatal appointments.
- Transmission from mom isn’t the only way babies get it. Some reports suggest that infants may catch it from other family members, such as fathers who carry the virus. Family members aren’t routinely screened, so these infections would be missed.
The simplest and best answer we have is to look back at history. Before the hepatitis B vaccine was recommended for all infants, about 18,000 babies and children caught hepatitis B every year. Half of them caught it from their mom, and the other half had no clear source of infection — they may have caught it from another family member, someone at daycare, or some other source. If we only give the vaccine when moms screen positive, we’ll miss those 9,000 kids who had no known risk factor but still caught it.
What are the risks of immunization?
The hepatitis B vaccine has a strong safety profile, but like every medicine and vaccine, there are some rare risks. The most serious known risk for hepatitis B immunization is allergic reaction: about 1 in 600,000 infants who are vaccinated develop anaphylaxis. Putting these numbers in context — if every one of the 3.5 million infants born in the US every year gets the shot, that comes out to about 6 cases of anaphylaxis per year (compare that to the 18,000 babies who caught hepatitis B before the vaccines was universally recommended). While anaphylaxis is serious, it’s also treatable, and babies are monitored after immunization for any signs of allergic reaction and treatment is given if needed.
What will happen if the birth dose is removed from the vaccine schedule?
The logistics of this are not immediately clear, as pediatric associations and even different states are working to create their own vaccine recommendations in anticipation of changes from RFK Jr’s new vaccine panel. But that panel holds a lot of power, and it’s possible that if they remove the hepatitis B vaccine dose at birth from their recommended schedule, it could limit access for mothers who want it for their newborns. If that happens, history tells us more babies will catch hepatitis B and go on to develop serious liver disease later in life.
Not a good plan.
Kristen Panthagani, MD, PhD, is completing a combined emergency medicine residency and research fellowship focusing on health literacy and communication. In her free time, she is the creator of the newsletter You Can Know Things, available on Substack and youcanknowthings.com. You can also find her on Instagram and Threads. Views expressed belong to KP, not her employer.